Surgical management of nasal airway obstruction may include nostrils, columnella, nasal (luminal) valve, hypertrophied turbinates, soft and hard palate, tori, uvula, tongue, adenoids and tonsils.
Nostrils and Columella
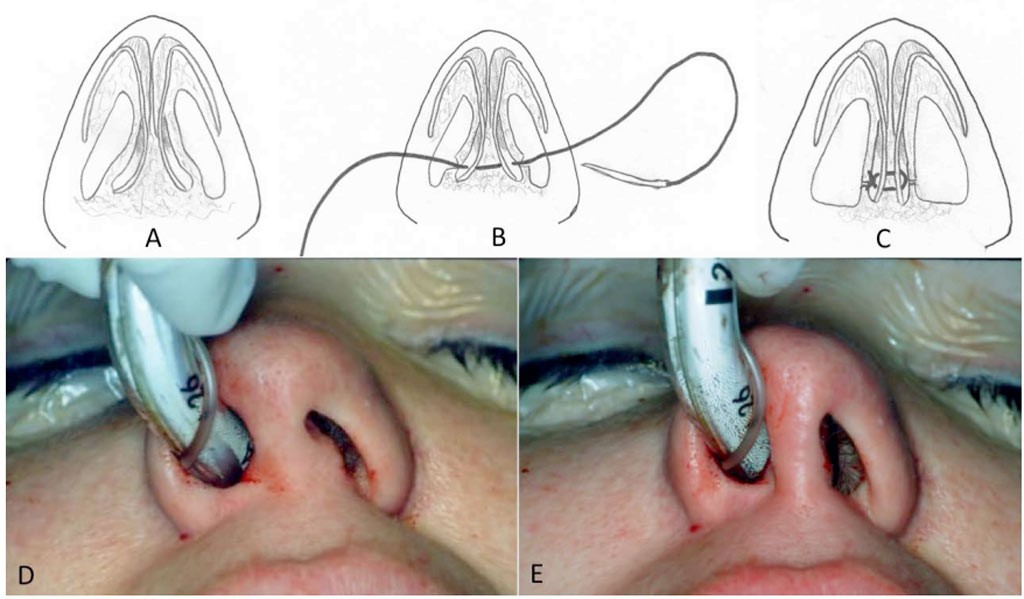
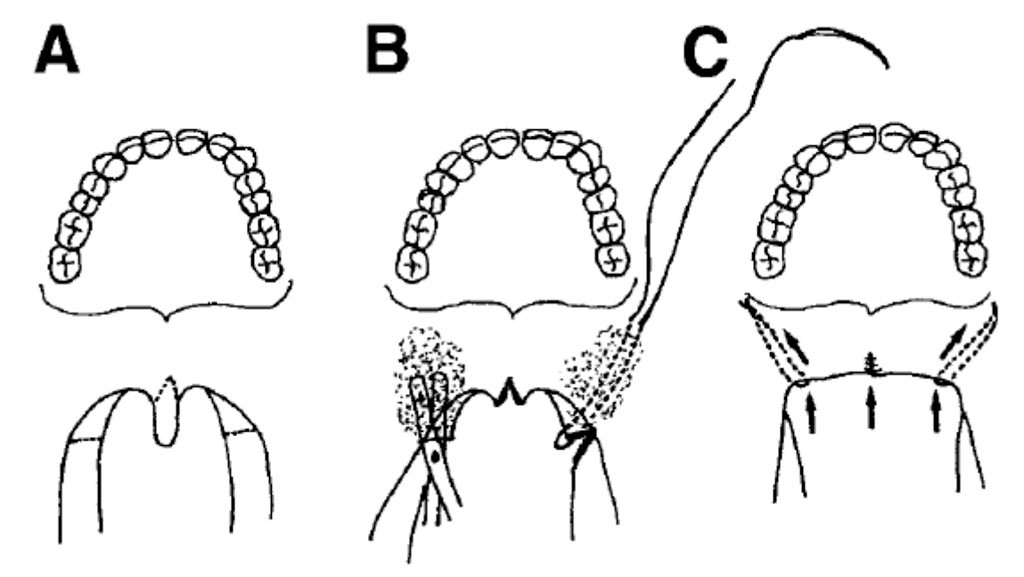
Many patients who have narrow nostrils have a wide columella. A relatively simple technique to reduce the transverse width of the columella can be employed to open the nostrils. The columella cinch suture technique is a method to narrow the columella and widen the nostril (Figure 1). The flared feet of the medial cruae are pulled together with a permanent 5.0 prolene suture t narrow the columella.
In addition, osteotomies to advance the maxilla forward will also widen the nostrils but will not affect the width of the columella.
FIGURE 1: (A-C) Illustration of columella cinch suture using a mattress suture with 5-0 clear Prolene placed through small incisions over the lateral feet of the medial cruae in order to decrease the width of the columella and increase the width of the nostrils, (D) Preapplication of columella cinch suture. (E) Post application of the cinch suture, narrowing the columella and widening the nostrils.
Luminal (Nasal) Valve
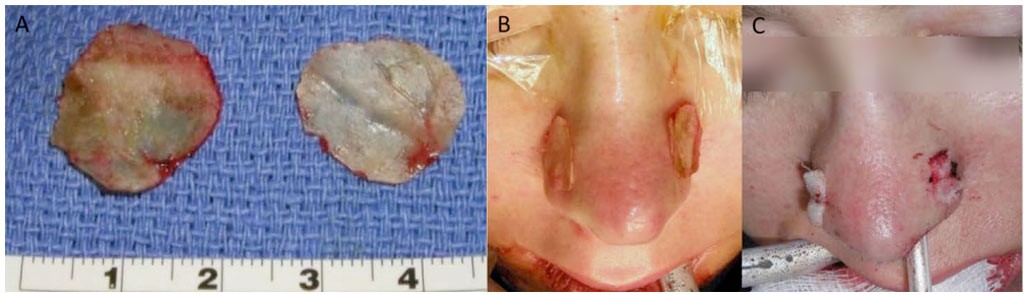
Luminal (nasal) valves may be constricted, and partially or completely block the nasal airway passage, particularly on inspiration. Soft tissue procedures can be performed to enlarge and expand the luminal valves to allow easier passage of air by tissue resection and multiple z-plasties with or without tissue grafting. Transverse nasal collapse is seen when the upper and lower lateral cartilages are deficient in substance or over-resection of the cartilages during rhinoplasty.
Thus, the lateral nasal walls collapse inward towards the septum and turbinates with inspiration obstructing the nasal airway. Batten grafts can be used to bolster up the width of the nose and give it more substance and firmness so that during inhalation the nostrils do not collapse and close off the nasal airway (Figures 2 and 3).
FIGURE 2: (A) Harvested bone from septum or posterior maxillary walls. (B) Prior to adaptation, and (C) Application of Batten graft inserted through internasal incisions to prevent transverse nasal collapse and stabilize with temporary sutures over for 5 to 7 days.
FIGURE 3: (A) Presurgery image of a patient with weak transverse cartilaginous stability, (B) Same patient 1 year after application of Batten graft, resulting in increased substance and firmness of the nose, preventing its collapse with inspiration.
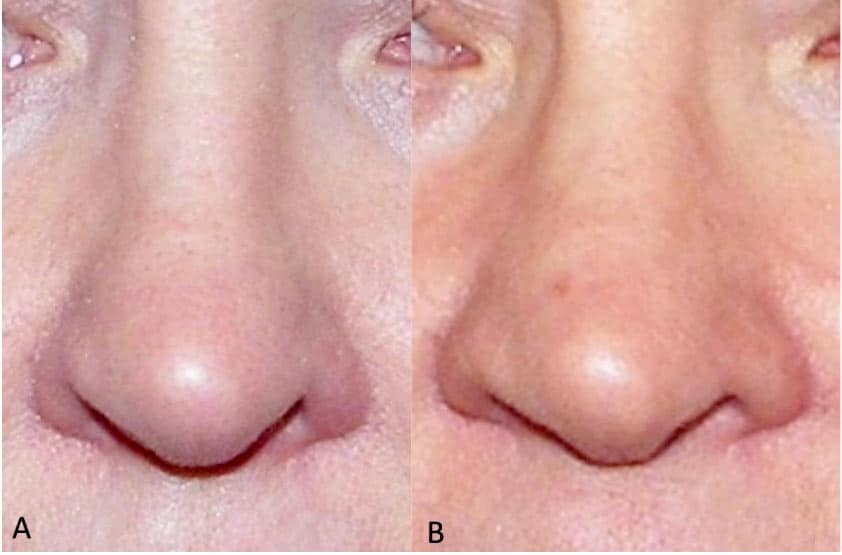
Hypertrophied Turbinates
Hypertrophied turbinates commonly contribute to nasal airway obstruction. When performed as an independent procedure, there are a number of techniques that can be used to reduce the turbinates. The most predictable is a partial resection of the turbinates. This can be done intranasally as well as when maxillary osteotomies are performed and the maxilla is down fractured and mobilized. This provides direct access to the turbinates after incising through the mucoperiosteum of the nasal floor to expose the turbinates (Figure 4).
The turbinates can easily be resected from the most anterior to the most posterior aspect of the nasal cavity under direct visualization. Usually about two-thirds of the turbinates can be resected and removed. For septal deviation, while the maxilla is down fractured, there is direct access to the septum as well where deviations and septal spurs can be removed and the septum repaired and straightened.
FIGURE4: A and B) Presurgery axial and coronal cone beam computed tomography (CBCT) views of hypertrophied turbinates with significant nasal airway obstruction. C and D) Postsurgery axial and coronal CBCT of the same patient, 2 years postsurgery.
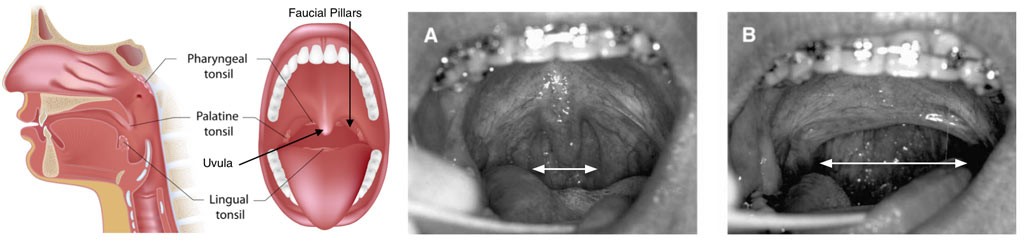
Uvulopalatopharyngoplasty (UPPP)
The UPPP is a technique to reduce or eliminate the uvula as well as shorten the soft palate anteroposteriorly. The traditional UPPP methods usually involve the use of a laser or electric cautery removing the posterior portion of the soft palate and uvula. This technique unfortunately creates a severe burn to the tissues at the posterior border of the soft palate and consequently a scar band can form around the soft palate extending down into the fascial pillars.
This can cause a tethering effect on the soft palate, eliminating its functional mobility. If a patient continues to have sleep apnea, this procedure is often repeated, because the surgeon fails to recognize that the airway obstruction is commonly lower at the base of the tongue and not at the soft palate level. These repeated reductions in soft palate length could result in patients developing hypernasal speech quality and velopharyngeal incompetence. In this situation, the speech becomes nasal and food and drink can go into the nasal cavity upon swallowing.
The senior author developed a modified form of the UPPP procedure that protects and maintains the soft tissue at the posterior border of the soft palate, but shortens the uvula and soft palate by an inversion flap technique (Figures 5 and 6).6 This predictably shortens the A-P length of the soft palate and uvula, yet protects the soft palate tissue by eliminating scar tissue along the posterior border as well as provides a wider transverse width of the soft palate.
FIGURE 5: Diagram of the modified UPPP. A) Note the hypertrophic uvula and the narrow transverse dimension between the right and left faucial pillars. The incisions are outlined at the posterior faucial pillar bilaterally and at the base of the uvula. B) After completion of the incisions and removal of the majority of the uvula, dissection into the soft palate tissues is performed in a submucosal plane between the oral and nasal sides with right-angled scissors.
A horizontal mattress suture is passed submucosally from the base of the maxillary tuberosity out through the incision on the posterior faucial pillar. The suture is then passed in a mattress fashion through the dissected lateral flap on the posterior faucial pillar and then tunneled back to the maxillary tuberosity region. The sutures are then tightened to shorten the soft palate to the desired dimension. C) Postsurgical view of the velopharyngeal structures after a modified UPPP procedure.
FIGURE 6: A) Presurgery photograph showing hypertrophic uvula and the narrow transverse dimension between the right and left faucial pillars. B) Postsurgical photograph after modified UPPP. Note the increased transverse dimension of the oropharyngeal airway after lateralization and anterior repositioning of the posterior faucial pillars.
Macroglossia (Large Tongue)
When the tongue is too large, a reduction glossectomy can be performed that reduces the anterior and central portion of tongue (Figure 7). This can considerably reduce the volume of the tongue and allow it to sit further forward in the mouth, opening the oropharyngeal airway.
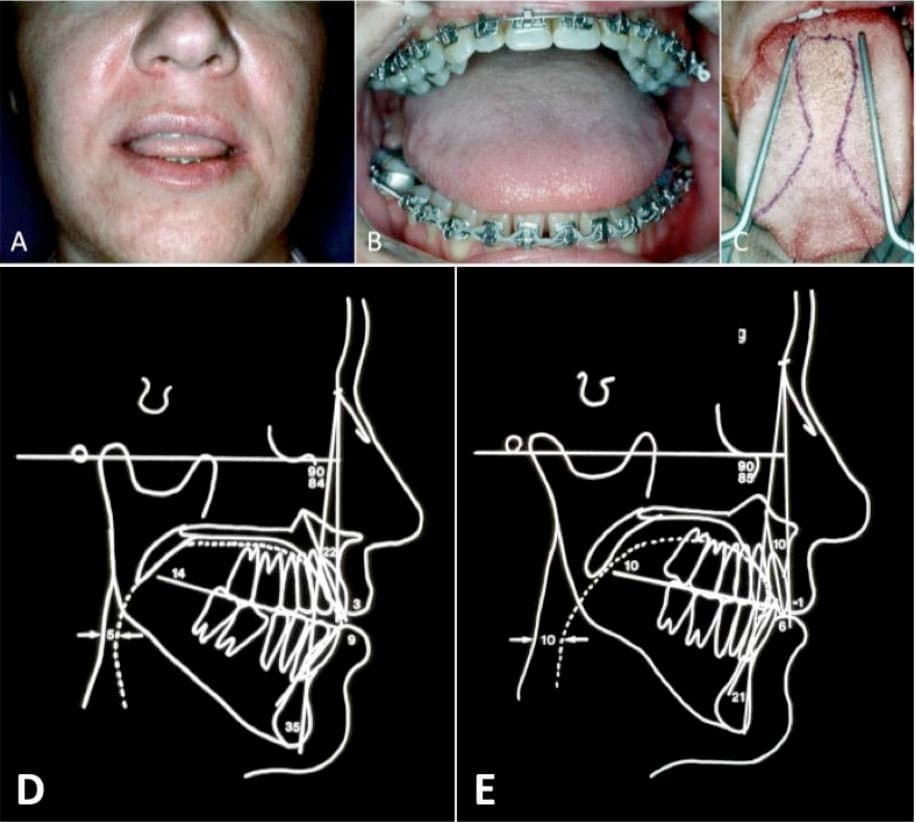
FIGURE 7: A) Macroglossia with tongue protruding through the anterior open bite, B) Large tongue overlapping lower teeth, C) Outline for reduction glossectomy. D) Presurgery lateral cephalogram illustrates the decreased oropharyngeal airway with an A-P dimension of 5 mm. E) Following a reduction glossectomy, the oropharyngeal airway increased to 10 mm.
Adjunctive Procedures
Additional techniques that have been used to try to open the airway include hyoid suspension, genioplasty, and advancement of the genial tubercles. Generally, these techniques do not help open the oropharyngeal airway very much because in many of these cases, there is no room for the tongue to move forward because the oral cavity volume remains unchanged.
Oftentimes, some of these ancillary methods (i.e. genioplasty) are done in conjunction with orthognathic surgical procedures where the maxilla and mandible are advanced that give a much higher predictability of opening the oropharyngeal airway.
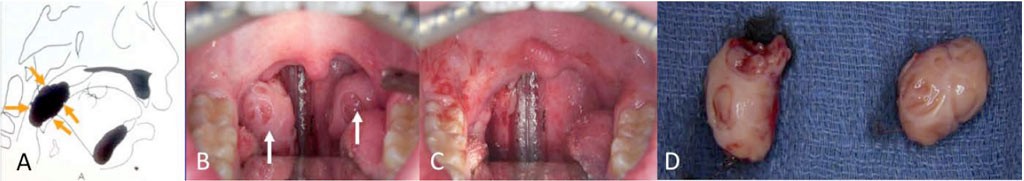
Tori of the Maxilla or Mandible
Mandibular and maxillary tori when excessively large can contribute to displacement of the tongue posteriorly. Removal of the lingual tori and palatal tori will increase the oral cavity volume allowing more oral cavity space to accommodate the tongue, thus, generally allowing it to sit further forward (Figure 8).
FIGURE8: A) Large mandibular tori (white arrows) can displace the tongue upwards and posteriorly, B) Space created by removal of the mandibular tori.
Tonsils and Adenoid Tissue
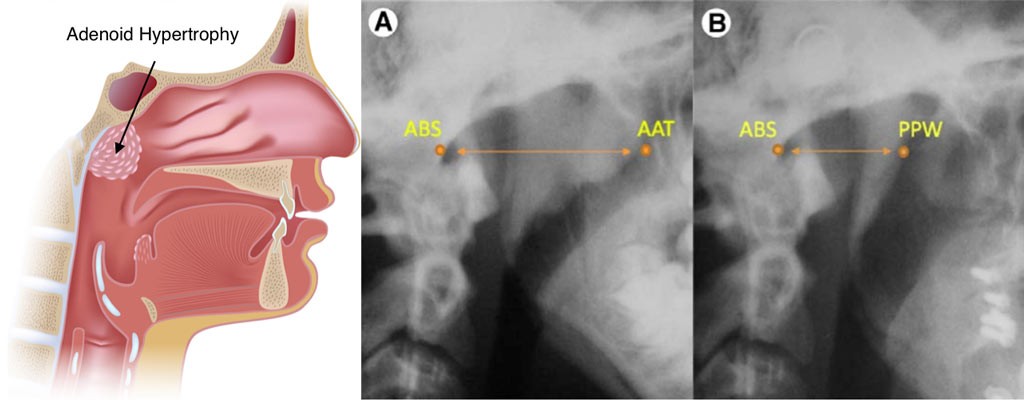
We have previously published a technique to remove the adenoid tissues through access with the Le Fort I osteotomy, approaching the adenoid tissue from above the hard and soft palates. 7
FIGURE 9: A) Hypertrophied tonsils can cause significant oropharyngeal airway obstruction, B) Intraoral view of hypertrophied tonsils, C) Tonsillectomy completed, D) Tonsil specimens.
FIGURE 10: Landmarks for measuring adenoid tissue; A) before surgery, B) After nasopharyngeal adenoidectomy. ABS, point at junction of atlas and base of skull; AAT, most anterior area of adenoid tissue; PPW, posterior pharyngeal wall.
Wolford et al. Airway Space Changes After Nasopharyngeal Adenoidectomy. J Oral Maxillofac Surg 2012.